Around eight in 10 deaths from breast cancer are in people who present to a healthcare professional with a symptom – this is why it’s so critical for detection to happen before there are signs of the disease.
For Jayne, who is a National Breast Cancer Foundation (NBCF) Community Ambassador, early detection saved her life.
Jayne was usually quite proactive with screenings and before a trip overseas last year, she was sent a reminder to get a routine mammogram so she arranged an appointment.
“I had no symptoms whatsoever,” she tells Women’s Agenda.
“I was happy, healthy, turned 50 in August and my son had turned 18, so we went on a sort of ‘coming of age trip’ together.”
After the screening, Jayne didn’t think much about it.
She and her son were having the trip of a lifetime and were spending time in Madrid when she received a text to contact BreastScreen.
BreastScreen is a national program funded by federal, state and territory governments, which offers free biennial mammograms to women over 40.
“Again, I didn’t think a great deal of it,” she says.
“I rang the clinic back and they said, ‘Look, no big deal – it’s pretty standard, some [people] we just like to double-check.”
She was also made aware that for every 1000 women who came through BreastScreen, around 50 have to get checked again and six end up being diagnosed with breast cancer.
Thinking her odds were fine, Jayne enjoyed the last few days of her holiday and went into the clinic once she returned to Australia.
Jayne took her husband as a support person but was reassured the appointment would just be a check-up.
After a touch test, more mammograms and an ultrasound, Jayne realised something was wrong.
“That was the point I knew I had breast cancer,” she says.
“There’s a lot to process really quickly. My husband flipped straight into denial and I went straight into death sentence. I was overwhelmed.”
Jayne was struck with dread about what would happen to her children and husband.
She was also worried about how she would manage her consulting business.
“There were just a million thoughts flooding through my head,” she says.
The past year has been a whirlwind of appointments, hospital visits and gruelling treatment, which included a lumpectomy and weeks of a type of chemotherapy nicknamed the ‘Red Devil’ for its harsh side effects.
“That’s a really nasty one,” says Jayne.
“I ended up back in hospital, had a couple of blood transfusions, the classic vomiting in the bucket at night. Nasty, nasty stuff, but it did its job.”
Jayne had to endure more weeks of another type of chemotherapy, but she was taken off it early after she experienced nerve damage to the side of her head.
She was finally able to complete treatment after three weeks of radiation.
She was also given a course of estrogen blockers that she was meant to be on for five years, but after feeling “zombified” for seven months, she made a quality-of-life decision with her doctor to come off them.
Reflecting on her journey, Jayne can’t stress enough the importance of breast screening for early detection.
As a community ambassador for NBCF, she encourages every woman in her life to stay on top of their breast screens and has shared her story in the hopes that our readers heed this advice.
She also actively fundraises for NBCF to help support its research and getting to Zero Deaths from the disease.
“Anything they can do to improve screening is just so critical because I would have never known,” says Jayne.
“Once the tumour got large enough, I may have felt it. But I was already at Stage 2, so if that tumour had to get bigger and it had to go through more lymph nodes, who knows where I’d be.”
Advancements in screening
National cancer screening programs are lifesaving.
But the same technology for breast screening has been used since the national initiative began more than three decades ago.

Research, backed by NBCF, could transform how breast screening is done in Australia in the future.
Dr Luke Marinovich is looking into 3D imaging and AI analysis to improve early detection.
He hopes these tools will address some of the limitations that come with traditional 2D mammograms.
“For every 1000 women who are screened, there might be seven cancers that are detected and there might be two that are missed that go on to present with symptoms later on – so there is certainly the opportunity to improve,” he tells Women’s Agenda.
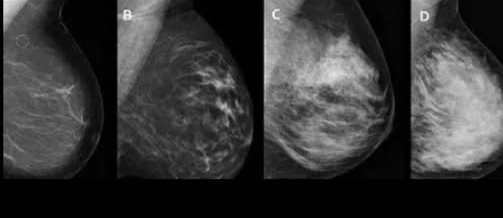
One key challenge with 2D mammography is that it can be difficult to spot cancer when a woman’s breast tissue is very dense.
These mammograms need to be read by at least two radiologists for any abnormal tissue to be identified.
But Dr Marinovich is researching the application of digital breast tomosynthesis (3D imaging) and AI analysis to make identifying breast cancer easier and faster.
His hope is to see these advancements implemented into population screening programs and to actively reduce the number of cancers missed.
“3D imaging takes not just one flat image but multiple images,” he says.
“It gives a much clearer depiction of the breast tissue and if a cancer is present.
“It really addresses the challenge with breast density. The work that we’ve done shows that 3D mammograms increase cancer detection for everyone regardless of breast density, but it particularly increases cancer detection in women with dense breasts.”
Dr Marinovich says using AI to read 3D scans could potentially reduce the amount of time it takes to find out if a person has breast cancer – but further research is needed.
“We’re working to establish whether AI is an accurate way of detecting cancer so that it can safely and efficiently be used,” he says.
Research like this could lead to some exciting breakthroughs in years to come and it would mean increasing the chances of early detection, treatment and survival for women like Jayne.
The National Breast Cancer Foundation (NBCF) funds world-class breast cancer research to prevent, detect, stop and treat this disease – research that ultimately saves lives.

