We’ve explained that the conditions being created by this health crisis, with its impacts upon people’s job security, incomes and caring responsibilities, and citizens being told to “stay at home” will create a perfect storm for families already plagued by abuse.
We pointed to experience overseas which showed a spike in domestic violence cases as the COVID-19 crisis hit. Now we’re starting to see it play out in Australia, with increased client numbers and more complex cases coming through our doors at the frontline.
But have we been calling for an increased investment in mental health services to respond to this urgent crisis? No. For a number of reasons.
Mental illness is not a key driver of domestic and family violence. In a recent study undertaken by the Kirby Institute, 492,393 domestic violence police events were examined over a 12-year period for associated mental health links, and only 15.83% came up positive.
In fact, what we know is, someone with a mental illness is much more likely to be a victim of domestic violence rather than a perpetrator.
So why, then, are we not calling for an urgent injection of funds into mental health services for domestic violence victims at this time? Well, it’s a bit like Maslow’s Hierarchy of Needs.
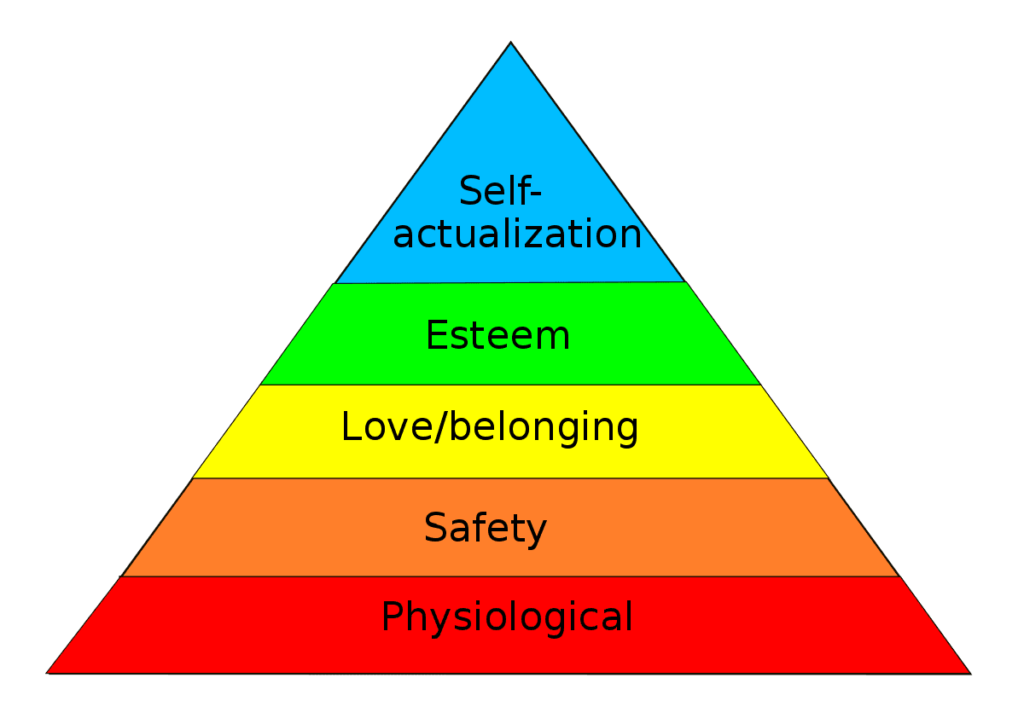
The priority right now is in ensuring women and children can actually escape the violence and abuse they are experiencing and have support and protections in place to remain safely in their homes, or to move to more suitable accommodation.
Aside from initial disclosures and violence-informed support throughout the case management process, most women and children won’t be ready to engage in in-depth counselling so as to heal and recover from the trauma of violence and abuse experienced until they are actually safe.
Why does it matter? Aside from the fact that we urgently need resources to flow into the areas at the bottom of Maslow’s Hierarchy – the case management support, housing options and legal assistance domestic violence victims need to be safe – erroneously focusing on mental health services as a response to domestic violence acts to reinforce misconceptions in the community about what actually drives violence against women.
What is often suggested in media reporting and public discourse around particular cases of domestic violence is that men who use violence and abuse against their partners and children must be mentally ill.
This can be a palatable way of thinking about men’s violence against women and children as we are able to “other” the offender in a manner that does not require us to confront the commonality of domestic violence nor the underlying societal conditions which support it; societal conditions that other men, non-violent men, also benefit from.
These, as we know are gender inequalities underpinned by rigid gender stereotypes, men’s control of decision-making, limits to women’s independence in public life and relationships, male peer relationships that emphasise aggression and disrespect towards women, and out-and-out condoning or excusing of men’s violence against women.
So, what if we don’t confront these realities head on? What if we keep conflating domestic violence with mental health? It will mean we are not putting our finite resources towards tackling the scourge of domestic violence in this country to where they are most needed first.
And it will also mean that we, as a society, continue to underestimate the scale of the problem and its relatability to all of us. This causes us to de-prioritise it and put less resources into tackling the problem than we actually need. And the cost? The safety of thousands upon thousands of Australian women and children who are currently trapped in violent and abusive households.
Let’s then ensure we fund mental health services at this time, for they are indeed crucial as the country faces the stresses and changes associated with the COVID-19 pandemic. But, when it comes to tackling domestic violence, please don’t bang on about mental health interventions.
Please listen to the experts and support our calls for adequate funding for the critical services and interventions we know women and children need to achieve safety.

